What is Stenting?
Stenting, particularly coronary stenting, is a common and essential procedure in modern cardiology. This procedure helps to open narrowed or blocked coronary arteries, ensuring better blood flow to the heart. Understanding what stenting is, how it is performed, and its benefits and risks can help patients make informed decisions about their heart health.
What is the process of understanding stenting?
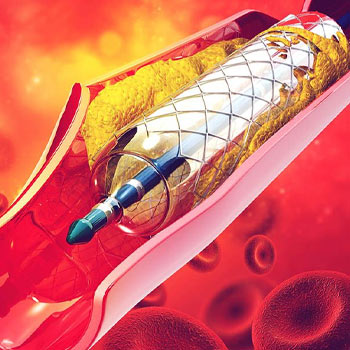
Stenting involves the placement of a small, mesh-like tube called a stent into a narrowed or blocked artery. This tube helps to prop the artery open, preventing it from narrowing again and ensuring adequate blood flow. Stenting is often performed during a procedure called angioplasty, which involves the use of a balloon to widen the artery before placing the stent.
What is the procedure for coronary angioplasty and stenting?
Preparation and Anesthesia
The patient is usually given a mild sedative and a local anesthetic to numb the area where the catheter (a thin, flexible tube) will be inserted, typically in the groin or arm.
Catheter Insertion
The cardiologist inserts the catheter into the artery and guides it to the heart using X-ray imaging.
Angioplasty
A small balloon at the tip of the catheter is inflated at the site of the blockage, compressing the plaque against the artery walls and widening the artery.
Stent Placement
Once the artery is widened, the stent is placed in the artery to keep it open. The stent is often mounted on the balloon, so when the balloon is inflated, the stent expands and locks into place.
Final Steps
The balloon is deflated and removed, leaving the stent in place. The catheter is then withdrawn, and pressure is applied to the insertion site to prevent bleeding.
Types of Stents
There are two main types of stents used in coronary stenting
Bare-Metal Stents
These stents are made of metal and do not have any special coatings. They provide a scaffold to keep the artery open but have a higher risk of restenosis (re-narrowing of the artery) compared to drug-eluting stents.
Drug-Eluting Stents
These stents are coated with medication that slowly releases into the artery to prevent the growth of scar tissue. This helps to reduce the risk of restenosis.
Benefits of Stenting
Restores Blood Flow
Stenting helps to restore proper blood flow to the heart, reducing symptoms like chest pain (angina) and improving the patient's quality of life.
Minimally Invasive
Compared to coronary artery bypass surgery, stenting is a less invasive procedure with a shorter recovery time.
Reduces Risk of Heart Attack
By opening blocked arteries, stenting can reduce the risk of a heart attack in patients with significant coronary artery disease.
Immediate Results
Patients often experience immediate relief from symptoms after the procedure.
Post-Procedure Care
Medication
Patients are typically prescribed antiplatelet medications (such as aspirin and clopidogrel) to prevent blood clots. It's crucial to follow the medication regimen as prescribed by the cardiologist.
Lifestyle Changes
Adopting a heart-healthy lifestyle can improve the long-term success of the stent. This includes a balanced diet, regular exercise, quitting smoking, and managing stress.
Regular Check-Ups
Follow-up appointments with the cardiologist are essential to monitor the patient’s heart health and ensure the stent is functioning properly.
When is Stenting Recommended?
Stenting is recommended for patients with significant coronary artery disease, particularly those who have
- Severe Angina: Persistent chest pain that is not relieved by medication or lifestyle changes
- Heart Attack: During or after a heart attack to open a blocked artery and restore blood flow
- Blocked Coronary Arteries: Identified through diagnostic tests such as angiography, which shows significant narrowing or blockages in the arteries
- Failed Medical Therapy: When medication and lifestyle changes have not successfully managed symptoms or improved heart health.
Stenting is a vital procedure in the field of cardiology, offering a minimally invasive solution to restore blood flow in blocked coronary arteries. While the procedure carries some risks, its benefits in improving heart health and quality of life are significant. Patients undergoing stenting should follow their cardiologist’s advice on medication, lifestyle changes, and regular follow-ups to ensure the best possible outcomes. Understanding what stenting involves and how it can help manage coronary artery disease empowers patients to take an active role in their heart health.
