What is Angioplasty?
Angioplasty, also known as percutaneous coronary intervention (PCI), is a minimally invasive procedure used to open up narrowed or blocked arteries, typically caused by coronary artery disease (CAD). This procedure is vital in restoring blood flow to the heart, alleviating chest pain (angina), and preventing heart attacks. Angioplasty has become a common and life-saving treatment for many patients with cardiovascular diseases. In this guide, we will explore what angioplasty is, the types, the procedure, its benefits, risks, and recovery process.
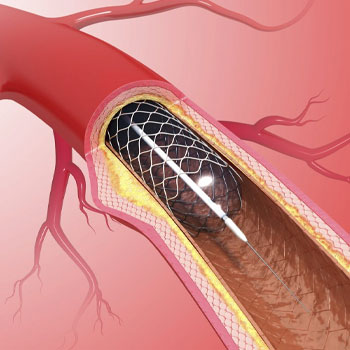
Angioplasty involves the use of a catheter—a thin, flexible tube—that is inserted into a blood vessel, typically in the groin or wrist, and guided to the site of the blockage in the coronary arteries. Once in place, a balloon at the tip of the catheter is inflated to compress the plaque against the artery wall, thereby widening the artery and restoring blood flow. In many cases, a small wire mesh tube called a stent is also placed in the artery to keep it open after the balloon is deflated and removed.
Types of Angioplasty
There are several types of angioplasty procedures, each designed for specific conditions
Balloon Angioplasty
The most common type, where a small balloon is inflated inside the artery to push the plaque against the artery walls, widening the vessel.
Stent Placement
Often performed in conjunction with balloon angioplasty. A stent (a small, mesh tube) is inserted into the artery to keep it open after the balloon is removed. Stents can be bare-metal or drug-eluting, which slowly release medication to prevent re-narrowing.
Atherectomy
Involves removing plaque from the artery using a catheter with a rotating shaver or laser. This is typically used when the plaque is hard and calcified.
Cutting Balloon Angioplasty
Uses a balloon with small blades to cut through the plaque, allowing the artery to widen.
The Angioplasty Procedure
The angioplasty procedure involves several steps and is usually performed by an interventional cardiologist in a catheterization laboratory (cath lab).
Preparation
The patient is given a local anesthetic to numb the area where the catheter will be inserted, usually the groin, wrist, or arm. Sometimes, a sedative is provided to help the patient relax.
Insertion of the Catheter
A small incision is made, and a sheath is inserted into the artery. Through this sheath, a thin, flexible tube called a catheter is guided to the coronary arteries. This process is monitored using real-time X-ray images (fluoroscopy).
Balloon Inflation
Once the catheter reaches the narrowed area, a smaller balloon catheter is threaded through it to the site of the blockage. The balloon is then inflated, compressing the plaque against the artery walls and widening the artery
Stent Placement
If a stent is required, it is mounted on the balloon catheter and positioned at the blockage site. When the balloon is inflated, the stent expands and locks into place, creating a scaffold to keep the artery open.
Completion
The balloon is deflated and removed, leaving the stent in place (if used). The catheter is then withdrawn, and the incision site is closed.
Benefits of Angioplasty
Angioplasty offers numerous benefits, particularly for patients with coronary artery disease
Improved Blood Flow
By opening narrowed arteries, angioplasty restores adequate blood flow to the heart muscle, reducing chest pain and improving overall heart function.
Reduced Risk of Heart Attack
By treating blockages before they cause significant damage, angioplasty helps prevent heart attacks.
Minimally Invasive
Compared to traditional open-heart surgery, angioplasty is less invasive, involves smaller incisions, and has a quicker recovery time.
Quick Recovery
Most patients can return to normal activities within a week after the procedure
Symptom Relief
Angioplasty can quickly relieve symptoms of chest pain and shortness of breath, improving the quality of life.
Recovery and Aftercare
Recovery from angioplasty typically involves a short hospital stay, followed by a period of home rest and gradually resuming normal activities.
- Hospital Stay: Most patients stay in the hospital for 1-2 days after the procedure for monitoring
- Medications: Patients are prescribed medications, including antiplatelet drugs to prevent blood clots and other medications to manage risk factors like high blood pressure and high cholesterol.
- Lifestyle Changes: Adopting a heart-healthy lifestyle is crucial. This includes a balanced diet, regular exercise, quitting smoking, and managing stress.
- Follow-Up Care: Regular follow-up appointments with a cardiologist are essential to monitor heart health and the success of the procedure.
- Cardiac Rehabilitation: Many patients benefit from a structured cardiac rehabilitation program, which provides supervised exercise, education, and support to improve heart health.
Angioplasty is a highly effective procedure for treating coronary artery disease and preventing serious cardiovascular events. By understanding the types, procedure, benefits, risks, and recovery process, patients can make informed decisions about their heart health. If you experience symptoms of heart disease or have been diagnosed with coronary artery disease, consult with your healthcare provider to discuss whether angioplasty is a suitable treatment option for you. Early intervention can significantly improve outcomes and enhance the quality of life for those with cardiovascular conditions.
