In the realm of cardiology, the term "Permanent Pacemaker" often surfaces in discussions about managing heart rhythm disorders. This advanced medical device plays a pivotal role in restoring and regulating the heart's natural rhythm, ensuring optimal cardiovascular function. Let’s delve into what a Permanent Pacemaker is, how it works, its benefits, and its significance in modern cardiology.
What is a Permanent Pacemaker?
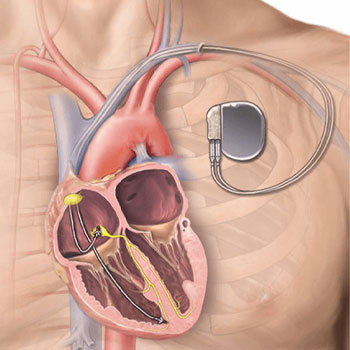
A Permanent Pacemaker is a small electronic device implanted under the skin, typically near the collarbone, to help control abnormal heart rhythms (arrhythmias). It consists of a pulse generator and leads (wires) that connect the device to the heart. Unlike temporary pacemakers used short-term in hospital settings, permanent pacemakers are designed for long-term use, often for several years.
How Does a Permanent Pacemaker Work?
The primary function of a Permanent Pacemaker is to monitor the heart’s electrical activity continuously and intervene when irregularities occur. Here’s a simplified breakdown of its operation
- Sensing: The pacemaker constantly monitors the heart’s electrical signals.
- Detection: It identifies abnormal heart rhythms or pauses in heartbeats
- Response: Upon detecting an irregularity, the pacemaker sends electrical impulses through the leads to the heart muscle, stimulating it to beat at a normal rate.
These impulses are mild and not typically felt by the individual. They simply prompt the heart to beat when its natural pacemaker (the sinoatrial node) fails to maintain a regular rhythm.
Conditions Requiring a Permanent Pacemaker
Permanent Pacemakers are primarily used to treat conditions such as
- Bradycardia: A slow heart rate that can lead to dizziness, fatigue, and fainting.
- Heart Block: A condition where the electrical signals from the atria (upper chambers of the heart) do not reach the ventricles (lower chambers) properly.
- Tachy-brady Syndrome: A combination of fast and slow heart rhythms that alternate irregularly.
- Heart Failure: In some cases, where heart failure is accompanied by arrhythmias that require pacing support.
Types of Permanent Pacemakers
There are several types of permanent pacemakers tailored to individual patient needs
Single-Chamber Pacemakers
These devices have one lead connected either to the atrium or ventricle.
Dual-Chamber Pacemakers
With leads in both the atrium and ventricle, these pacemakers coordinate the timing of contractions between the chambers more closely.
Biventricular (or Cardiac Resynchronization) Pacemakers
Used in heart failure patients, these devices stimulate both ventricles simultaneously to improve synchronization and pump efficiency.
The type recommended depends on the specific heart condition and the electrical needs of the patient.
Benefits of Permanent Pacemakers
Improved Quality of Life
Pacemakers alleviate symptoms associated with irregular heart rhythms, such as fatigue and fainting, allowing individuals to resume normal activities.
Risk Reduction
By maintaining a regular heartbeat, pacemakers lower the risk of complications like stroke and heart failure.
Long-Term Support
Designed to last several years, pacemakers provide sustained cardiac support and can be adjusted as needed through non-invasive programming.
Implantation Procedure and Recovery
The implantation of a Permanent Pacemaker is typically performed under local anesthesia in a hospital setting. The procedure involves making a small incision near the collarbone, inserting the leads into a vein, and guiding them to the heart. The pacemaker generator is then placed under the skin and connected to the leads. Recovery time is minimal, with patients often able to return home the same day or within a day after surgery. Regular follow-up visits ensure the pacemaker functions optimally and can be adjusted if necessary.
Living with a Permanent Pacemaker
Living with a pacemaker generally requires few lifestyle adjustments. While certain precautions may be advised, such as avoiding strong magnetic fields and undergoing regular check-ups, most individuals can lead active, fulfilling lives. Routine activities, including exercise and travel, are usually permissible once the implant site has healed.
Future Developments and Innovations
Advancements in pacemaker technology continue to enhance their effectiveness and longevity. Innovations such as leadless pacemakers, which do not require leads implanted in the heart, and remote monitoring capabilities are expanding treatment options and improving patient care.
In conclusion, a Permanent Pacemaker is a sophisticated yet essential device in modern cardiology, offering reliable support for individuals with various heart rhythm disorders. By regulating heartbeats and mitigating associated symptoms, pacemakers significantly enhance quality of life and reduce health risks. As technology evolves, these devices continue to evolve, promising even greater benefits and improvements in cardiac care.
For anyone living with a heart condition requiring rhythm management, consulting a cardiologist about the potential benefits of a Permanent Pacemaker can provide valuable insights and personalized care options.
