Peripheral angioplasty is a minimally invasive procedure used to treat narrowed or blocked arteries outside the heart, typically in the legs. This procedure is crucial in managing peripheral artery disease (PAD), a condition where arteries in the extremities become narrowed or blocked due to the buildup of plaque a condition that can lead to reduced blood flow, pain, and potential tissue damage if left untreated.
What Is Peripheral Angioplasty?
Peripheral angioplasty involves the following key steps
Diagnostic Evaluation
Before the procedure, a thorough evaluation of the patient's condition is conducted. This includes medical history review, physical examination, and diagnostic tests such as ultrasound, CT angiography, or magnetic resonance angiography (MRA) to locate and assess the extent of the blockage.
Procedure Setup
The patient is typically given local anesthesia at the site of arterial access, often in the groin or wrist. A small puncture is made in the skin, through which a catheter (a thin, flexible tube) is inserted into the artery.
Guidewire Placement
Using fluoroscopic guidance (real-time X-ray imaging), a guidewire is threaded through the catheter to reach the narrowed or blocked artery in the leg.
Balloon Inflation
A balloon-tipped catheter is advanced over the guidewire to the site of the blockage. Once in position, the balloon is inflated, compressing the plaque against the artery walls and widening the artery lumen to restore blood flow.
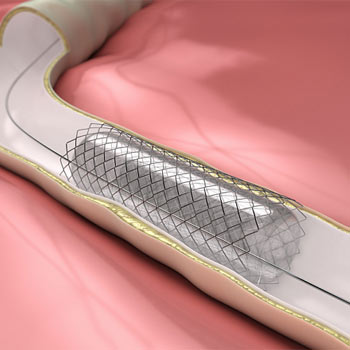
Stent Placement (if necessary)
In some cases, a stent—a small mesh tube—may be inserted and expanded at the site of the blockage to help keep the artery open. This is called a stenting procedure and may be performed concurrently with angioplasty.
Completion and Recovery
After the procedure, the catheter and guidewire are removed, and pressure is applied to the puncture site to prevent bleeding. Patients are typically monitored for a short period to ensure there are no complications before being discharged home.
Benefits of Peripheral Angioplasty
Improved Blood Flow
By opening up the blocked artery, peripheral angioplasty restores blood flow to the affected area, reducing symptoms such as leg pain and cramping during walking or at rest.
Minimally Invasive
Compared to traditional open surgery, angioplasty is minimally invasive, involving smaller incisions, less risk of infection, and quicker recovery times.
Customized Treatment
The procedure can be tailored to each patient's specific anatomy and condition, allowing for precise treatment of multiple arterial blockages if necessary.
Reduced Risk
Peripheral angioplasty carries lower risks of complications compared to surgical alternatives, making it a preferred option for many patients.
Recovery and Follow-Up
Following peripheral angioplasty, patients are usually advised to take it easy for a short period, avoiding strenuous activities. Medications to prevent blood clots and manage underlying conditions such as high blood pressure or diabetes may be prescribed. Regular follow-up appointments and lifestyle modifications (such as smoking cessation and dietary changes) are essential to maintain the benefits of the procedure long-term.
Peripheral angioplasty is a valuable procedure in the management of peripheral artery disease, offering patients relief from symptoms and improving overall quality of life. As with any medical intervention, it is important for individuals to consult with healthcare providers to determine the most appropriate treatment plan based on their specific condition and medical history.
By understanding the basics of peripheral angioplasty, patients and caregivers can make informed decisions about their healthcare journey, ensuring optimal outcomes and improved vascular health.
